
NYSTATIN SWISH FREE
In Meyler's Side Effects of Drugs (Sixteenth Edition), 2016 Drug administration Drug formulationsĪfter it was shown that a liposomal formulation of nystatin had similar in vitro antifungal activity to a wide range of organisms as the free compound, an intravenous multilamellar liposomal formulation of nystatin was developed, but was subsequently withdrawn by the manufacturers.
NYSTATIN SWISH FULL
In some studies, fluconazole was changed to enteral administration when patients achieved full enteral feedings, and intravenous access was discontinued in order to complete 4-6 weeks of prophylaxis. For these reasons and to prevent colonization of central venous catheters, the intravenous route is recommended for fluconazole prophylaxis in preterm infants while peripheral or central intravenous catheters are present. It is during these patient conditions that fungal colonization, proliferation, and dissemination are likely to occur. Additionally, as discussed above, oral mucosa can be treated but enteral prophylaxis may not always be able to be given if patients have an ileus, NEC, intestinal perforation, or hemodynamic instability.


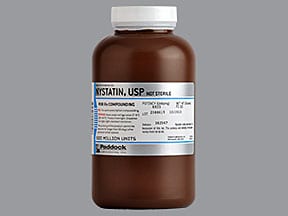
Although enteral fluconazole is 90% absorbed, absorption characteristics in preterm infants are variable and not well studied. Whereas oral fluconazole for prophylaxis was used in one of the above studies, almost all other fluconazole prophylaxis studies have used intravenous administration in the first weeks. Although a previous study had raised concerns regarding nystatin use and NEC and all-cause mortality, 110 this study demonstrated no difference between both groups regarding NEC (fluconazole 8.6%, nystatin 9.6%, placebo 9.9%) or mortality (fluconazole 8.6%, nystatin 8.5%, placebo 12.1%). Invasive Candida infections were significantly lower in both the fluconazole (3.2%) and nystatin (4.3%) groups compared with the placebo (16.5%) patients ( p <. This study demonstrated that nystatin prophylaxis resulted in decreased Candida colonization of the gastrointestinal tract, skin, and respiratory tract. 8 Patients were randomized (1:1:1) to fluconazole, nystatin, or placebo. Additionally, the oral suspension of nystatin has a very high osmolarity of 3002 mOsm/L, and there is a concern with the use of hyperosmolar medications and NEC.Īydemir et al., in a three-arm RCT of antifungal prophylaxis, compared intravenous fluconazole ( n = 93) and oral/enteral nystatin ( n = 94) with placebo ( n = 91) in infants less than 1500 grams. Nystatin is less efficacious compared to fluconazole and in one nystatin study a third of the eligible patients were excluded because of hemodynamic instability or gastrointestinal concerns. Some questions regarding fluconazole and nystatin prophylaxis remain unanswered, but there are two studies that have compared both agents.

Aydemir has demonstrated that nystatin (given 0.5 mL to the oral cavity and 0.5 mL via the feeding tube every 8 hours) decreases skin, gastrointestinal, and respiratory fungal colonization but not at other sites. Martin MBBS, FRACP, in Fanaroff and Martin's Neonatal-Perinatal Medicine, 2020 Fluconazole Versus Nystatin ProphylaxisĪntifungal prophylaxis with parenteral fluconazole is effective in preventing colonization of the skin, gastrointestinal and respiratory tracts, central venous catheter, and dissemination to multisite colonization ( Table 49.6), as well as eradicating colonization with Candida albicans, the most virulent yeast for preterm infants.


 0 kommentar(er)
0 kommentar(er)
